What Is Herd Immunity And What Does It Mean For COVID-19?
INDIVIDUAL IMMUNITY
Immunological memory is the ability of the immune system to quickly and specifically recognize a previously encountered antigen (i.e. a pathogen-derived epitope) and initiate a directed immune response. Generally, secondary, tertiary and subsequent immune responses are directed against the same antigen.While recent studies have shown the flexibility of the innate immune system, long-term protection against specific pathogens is largely attributed to the adaptive immune system, in particular, T cells and B cells. Immunological memory is sustained by long-lived antigen-specific lymphocytes that are induced by the original pathogen exposure. These clonally expanded populations persist in a quiescent state until they reencounter their cognate antigen. The ability of these cells to mount rapid and robust cell-mediated and/or antibody-mediated responses is critical to inhibiting and clearing secondary infections and thus provide immunity on an individual level.
HERD IMMUNITY
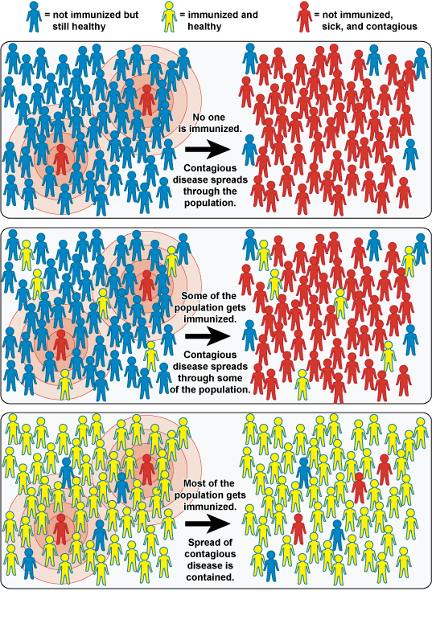
Now, this individual immunity is not only critical to human health and pathogen evolution, but can also scale up to a population level and impact the dynamics of pathogen transmission. Population-scale immunity is termed herd immunity and is the basis of many modern-day vaccination campaigns.
The National Institute of Allergy and Infectious Disease (NIAID)
In the theory of herd immunity, the percentage of a population that is immune to the specific-pathogen is the critical variable. Along with population density and transmission rate, the level of individual immunity in a population can be used to model pathogen transmission throughout a region or country. More importantly, this modeling helps determine the herd immunity threshold, which details the level of population immunity needed for the disease to no longer persist.
However, herd immunity isn’t as simple as three measurable variables. In actuality, there are hundreds of moving parts that influence herd immunity. These include factors at the cellular level as well and personal interaction dynamics at a population level.
For example, the ability of a pathogen or vaccine to elicit a robust primary immune response influences the quality of protection developed. Therefore, immunological memory is dependent upon the immunogenicity, context, epitopes and even co-infections that occur during the primary immune response. Additionally, because of these factors, the durability (i.e. length of protection) of immunological memory may vary between different individuals as well as different pathogens. This means that even if you were vaccinated as a child, your immunity may wane over time; thus the need for booster immunizations.
Bridging the gap between the individual and population, immunity derived from either natural infection or vaccines is only effective to the degree by which it limits onward transmission. This means that certain immunity can lessen the clinical symptoms of disease, thus protecting the individual. However, unless individual immunity limits pathogen transmission or carriage, it does not contribute towards the herd immunity threshold.
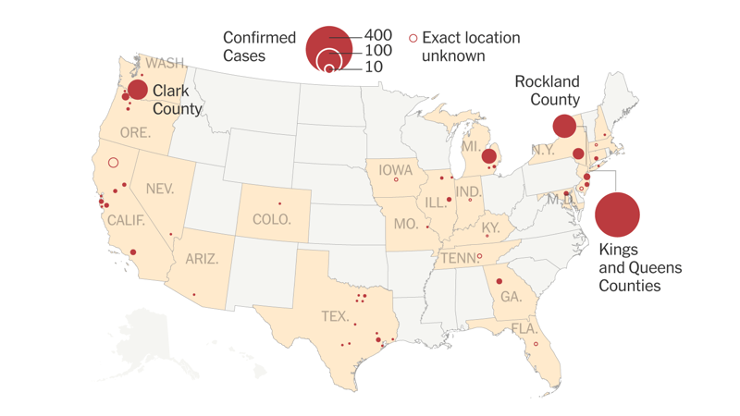
The New York Times
Finally, population level interactions can also influence herd immunity and patterns of pathogen transmission. Examples of this include high-birth-rate contexts, highly interconnected social demographics, as well as the concept of “free-loaders.” Non-compliance is partially attributed to religious exemptions, such as those seen in Orthodox Jewish communities. However, this emerging concept is most evident in the anti-vaccination movement, which withhold children from vaccination programs over fears of autism. As a result, this concentrated decline in immunity within particular demographics have led to numerous measles outbreaks, focused in California, Michigan, New York, Washington, Oregon.
As an example, measles is an interesting pathogen to characterize in the context of herd immunity, as measles has one of the highest transmission rates. This pathogen is so contagious, that in a population of naïve individuals, one person is expected to infect, on average, 15 people during the infectious period. Thus, the herd immunity threshold for measles is extremely high at approximately 93 to 95%. Since, the advent of the MMR vaccine in 1971, infection rates have remained low with 97% of people protected against measles, 88% against mumps, and at least 97% against rubella after two doses.
COVID-19 MODELING
So how does herd immunity relate COVID-19 and the current pandemic? As previously mentioned, immunity can be gained through either natural infection or vaccination. As detailed here, coronaviruses are actually fairly common and permeate through our population causing mild respiratory disease. Historically, SARS (2002) and MERS (2012) are the two most recent cross-species transmission events of coronaviruses, resulting in localized epidemics in China and the Arabian Peninsula.
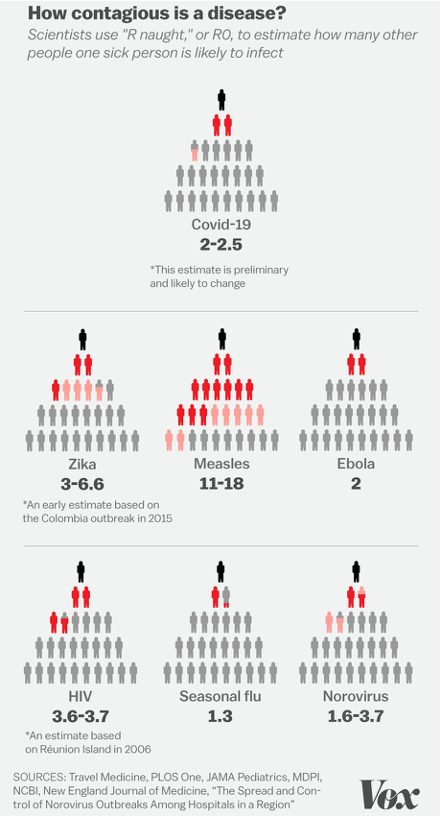
Javier Zarracina and Christina Animashuan — Vox
Based on developing data, the average transmission rate of COVID-19 is 2.5, but this rate is expected to change with more information. With isolation measures in place, transmission is likely to go down significantly. However, under normal circumstances, this is expected to place the herd immunity threshold for COVID-19 at ~70% population-level immunity. While the UK as well as Sweden, Norway and the Netherlands initially proposed building herd immunity through natural infections, these countries have formally backtracked and adopted social distancing policies. While natural immunity can be achieved through intentional exposure, as was previously done with chickenpox, COVID-19 carries a much higher risk of severe clinical disease and death. Many epidemiologists disagree with the use of herd immunity in the context of COVID-19, as there is no vaccine readily available.
UNANSWERED QUESTIONS
Further, questions still remain concerning individual immunity and the response that is evoked by natural infection with COVID-19. For a vaccine or natural infection against COVID-19 to contribute towards herd immunity, this immunity needs to follow similar rules as other pathogens such as measles, chickenpox and rubella. That is, infection by COVID-19 or a vaccine against COVID-19, must elicit a strongly immunogenic response in the proper context of inflammation against highly available epitopes. Additionally, the memory lymphocyte pool generated from the primary immune response must be long-lived and have the capacity to be robustly activated upon re-exposure to the virus.
As this is a novel virus, the fine molecular details that direct immunological memory against COVID-19 are completely unstudied and unraveling by the minute. Therefore, its critically important to understand the dynamics of these host-pathogen interactions and the development of long-lived immunity against COVID-19. In this way we can better inform vaccine development and the modeling of herd immunity for COVID-19.
About the Author
 Justin Moroney is a fourth year Ph.D. student in the molecular immunology and microbiology discipline of the Integrated Biomedical Sciences program. His research focuses on understanding and exploiting the molecular and regulatory underpinnings of human memory B cells to facilitate vaccine development. Outside of lab, Justin interns with UT Health San Antonio’s Office of Technology Commercialization and plays an active role in the scientific community as the program director of EnventureSA.
Justin Moroney is a fourth year Ph.D. student in the molecular immunology and microbiology discipline of the Integrated Biomedical Sciences program. His research focuses on understanding and exploiting the molecular and regulatory underpinnings of human memory B cells to facilitate vaccine development. Outside of lab, Justin interns with UT Health San Antonio’s Office of Technology Commercialization and plays an active role in the scientific community as the program director of EnventureSA.
References
Iftikhar, Noreen. “Herd Immunity: What It Means for COVID-19.” Healthline, Healthline Media, 2 Apr. 2020, www.healthline.com/health/herd-immunity.
Kwok, Kin On, et al. “Herd Immunity – Estimating the Level Required to Halt the COVID-19 Epidemics in Affected Countries.” Journal of Infection, 2020, doi:10.1016/j.jinf.2020.03.027.
Lindsay Smith Rogers, and JH Bloomberg School of Public Health. “What Is Herd Immunity and How Can We Achieve It With COVID-19?” Johns Hopkins Bloomberg School of Public Health, 14 Apr. 2020, www.jhsph.edu/covid-19/articles/achieving-herd-immunity-with-covid19.html.
Metcalf, C.j.e., et al. “Understanding Herd Immunity.” Trends in Immunology, vol. 36, no. 12, 2015, pp. 753–755., doi:10.1016/j.it.2015.10.004.
Meyerowitz-Katz, Gideon. “Here’s Why Herd Immunity Won’t Save Us From The COVID-19 Pandemic.” ScienceAlert, 2020, www.sciencealert.com/why-herd-immunity-will-not-save-us-from-the-covid-19-pandemic.
Prompetchara, Eakachai, et al. “Immune Responses in COVID-19 and Potential Vaccines: Lessons Learned from SARS and MERS Epidemic.” Asian Pacific Journal of Allergy and Immunology, 2020, doi:10.12932/ap-200220-0772.
Raoult, Didier, et al. “Coronavirus Infections: Epidemiological, Clinical and Immunological Features and Hypotheses.” Cell Stress, vol. 4, no. 4, 2020, pp. 66–75., doi:10.15698/cst2020.04.216.
Rashid, Harunor, et al. “Vaccination and Herd Immunity.” Current Opinion in Infectious Diseases, vol. 25, no. 3, 2012, pp. 243–249., doi:10.1097/qco.0b013e328352f727.
Resnick, Brian. “12 Things Everyone Needs to Know about the Coronavirus Pandemic.” Vox, Vox, 2 Apr. 2020, www.vox.com/science-and-health/2020/4/2/21197617/coronavirus-pandemic-covid-19-death-rate-transmission-risk-factors-lockdowns-social-distancing.